Key Benefits
- Check prostate health and BPH activity by measuring total and free PSA.
- Spot elevated PSA that flags enlargement or inflammation, not only prostate cancer.
- Clarify BPH versus cancer risk using percent-free PSA; higher values favor BPH.
- Guide next steps if PSA is high or percent-free low, including urology referral.
- Track trends and PSA velocity; rapid rises prompt imaging or biopsy discussions.
- Monitor response to finasteride or dutasteride; PSA typically halves within 6–12 months, and interpretation adjusts.
- Reduce false alarms by avoiding ejaculation, biking, infections, or retention before testing.
- Interpret best with age-specific ranges, prostate size, symptoms, and digital exam findings.
What are BPH
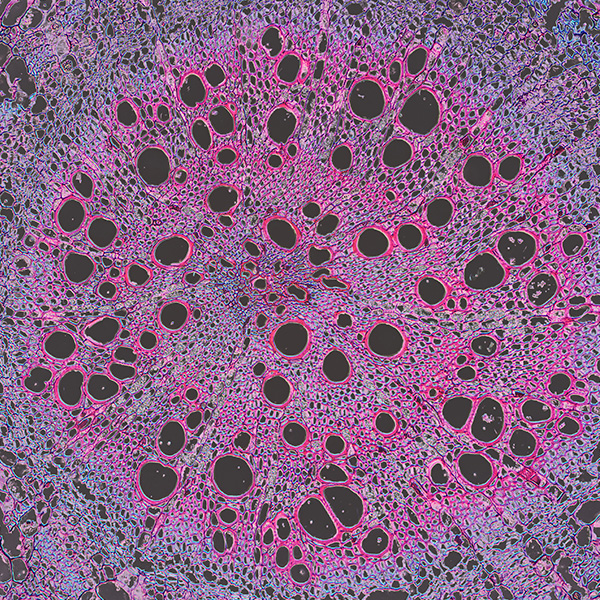
BPH biomarkers are measurable signals in blood or urine that reflect how the prostate is growing and how that growth affects the urinary tract. Most come from prostate cells and their secretions, so they mirror the gland’s activity and size; the best-known is a protein made by the prostate (prostate-specific antigen, PSA). As the prostate enlarges under hormone influence (dihydrotestosterone, DHT), more tissue and irritated ducts can release more of these signals into circulation. Biomarkers also capture the tissue’s response—such as low-grade inflammation—and the downstream strain on bladder outflow. In practice, testing helps estimate prostate burden without imaging, track whether the condition is stable or progressing, and gauge how well treatment is calming gland activity. Just as important, biomarker patterns help separate benign enlargement from other causes of similar symptoms, especially prostate cancer or infection, so care can be targeted and timely. In short, BPH biomarkers translate prostate biology into numbers that guide decisions.
Why are BPH biomarkers important?
BPH biomarkers translate what’s happening inside the prostate into signals about the whole urinary system. They help explain why a man’s stream weakens, why nights are interrupted by bathroom trips, and how bladder and even kidney function may be affected over time.
Total PSA is the most used marker; many labs consider values up to about 4 within reference, with age-adjusted upper limits rising toward 6–7 in older men. For prostate health, lower tends to be better. Clinicians also look at percent free PSA: higher percentages (often above about 25) lean toward benign enlargement, while lower percentages (around 10–15 or less) suggest a higher likelihood of malignancy rather than BPH. Context, age, and prostate size matter when interpreting these numbers.
When total PSA is low, it usually reflects a smaller gland with less leakage of PSA into the blood. Men in this range often have minimal obstruction: stronger flow, fewer nighttime awakenings, and less urgency. With aging, some may still notice urgency or frequency from bladder changes even if PSA stays low.
Higher total PSA often mirrors larger prostate volume or inflammation, which can slow flow, prolong voiding, and cause nocturia, infections, or, in severe cases, retention. If the percent free PSA is relatively high, that pattern fits BPH; if it’s low, cancer risk becomes the concern.
Big picture: these biomarkers sit at the crossroads of androgen biology, prostate growth, bladder dynamics, and kidney back-pressure. Tracked over time alongside symptoms, they help gauge long-term risks to urinary function, sleep quality, and overall well-being.
What Insights Will I Get?
Benign prostatic hyperplasia (BPH) reflects growth and remodeling of prostate tissue that can affect urinary flow, sleep quality, sexual function, and overall energy and cognition through nocturia and autonomic stress. Tracking BPH biomarkers helps index epithelial integrity, inflammatory tone, and androgen-responsive tissue activity—signals that ripple into cardiovascular and metabolic regulation. At Superpower, we test these specific biomarkers: PSA Total, Free PSA.
PSA (prostate‑specific antigen) is a protease made by prostate epithelial cells. In blood it circulates bound to proteins (complexed) and unbound (free). Total PSA reflects the overall leakage of PSA from the gland into circulation, which often rises with larger, more permeable prostates in BPH. The proportion that is unbound (Free PSA) tends to be higher in benign enlargement and lower when cell architecture is more distorted, as in many cancers.
For stability and healthy function, a steady, age‑appropriate Total PSA over time suggests relatively stable gland size and epithelial barrier function. When Total PSA is elevated, a higher Free‑to‑Total PSA proportion supports a benign, hyperplastic source; a lower proportion indicates greater concern for atypical remodeling and warrants closer clinical context. Together, these measures approximate prostate volume and tissue dynamics, signaling whether urinary tract load—and its downstream effects on sleep, cognition, and autonomic balance—is stable or shifting.
Notes: Interpretation varies by age, prostate size, and baseline trends. Ejaculation, cycling, prostatitis, urinary retention, recent instrumentation, and acute illness can transiently raise Total PSA. 5‑alpha‑reductase inhibitors lower PSA. Assay methods and biologic variation introduce small shifts; use the same lab and compare serially.






.avif)



.svg)





.svg)


.svg)


.svg)

.avif)
.svg)










.avif)
.avif)
.avif)


.avif)
.png)


