Key Benefits
- Confirm true calcium status and correctly adjust for albumin when assessing hypercalcemia.
- Spot hidden calcium imbalance when low or high albumin skews total calcium.
- Explain common symptoms like fatigue, constipation, thirst, or kidney stones from hypercalcemia.
- Guide next steps by prompting parathyroid hormone testing to pinpoint parathyroid-related causes.
- Protect bones, kidneys, and heart by flagging osteoporosis, stones, or arrhythmia risks.
- Support fertility and pregnancy by flagging risks to address before or during pregnancy.
- Track trends to gauge severity, medication effects, dehydration impact, and treatment response.
- Best interpreted with parathyroid hormone, vitamin D, kidney function, ionized calcium, and symptoms.
What are Hypercalcemia
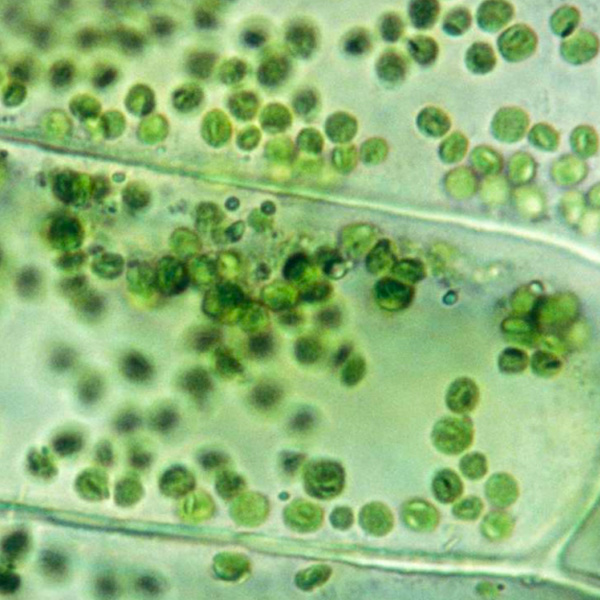
Hypercalcemia biomarkers are the key signals that confirm elevated calcium and reveal why it’s high. Testing begins with calcium itself, especially the biologically active form (ionized calcium), then looks at the hormones that set calcium balance: the parathyroid signal from the neck glands (parathyroid hormone, PTH), a tumor-associated mimic (parathyroid hormone–related peptide, PTHrP), and the vitamin D hormones made through skin, liver, and kidney steps—storage form (25-hydroxyvitamin D, 25(OH)D) and active form (1,25-dihydroxyvitamin D, calcitriol). These markers, read together, show whether excess calcium is being driven by over-signaling from parathyroid glands, tumor secretion, extra absorption from the gut, or release from bone. Companion findings such as the partner mineral (phosphate) and a bone formation enzyme (bone alkaline phosphatase, bone ALP) reflect how bone and kidneys are responding—whether calcium is being mobilized from the skeleton or retained/excreted. In short, hypercalcemia biomarker testing maps the body’s calcium-control network to pinpoint the source of imbalance and enable targeted care.
Why are Hypercalcemia biomarkers important?
Hypercalcemia biomarkers track how calcium moves through bone, kidneys, gut, and the nervous–cardiac system, under the pull of parathyroid hormone and vitamin D. They matter because calcium is both a structural mineral and an electrical signal; even small shifts alter muscle contraction, heart rhythm, cognition, and fluid balance.
Total calcium is generally about 8.5–10.2, with healthiest physiology clustering near the middle. Because much calcium rides on albumin, corrected calcium adjusts the total to estimate the biologically active (ionized) fraction; optimal also sits mid‑range. Albumin itself is typically 3.5–5.0; staying in the normal band helps total calcium reflect reality.
When values fall, two stories exist. A low total with normal corrected calcium points to low albumin, not true calcium lack—important, because low albumin can mask hypercalcemia. A genuinely low corrected (or ionized) calcium increases nerve and muscle excitability, bringing tingling, cramps, spasms, or seizures, and a prolonged QT on ECG; children may show irritability or tetany. In pregnancy, albumin naturally runs lower, so corrected calcium is the reliable lens.
When corrected calcium rises, hypercalcemia is present. Kidneys struggle to concentrate urine, leading to thirst and dehydration; stones may form. Gut motility slows, bones may ache, mood and clarity can drift to fatigue or confusion, and the QT interval shortens. Older adults may show cognitive change; children are prone to dehydration; in pregnancy, maternal complications (for example, stones) and neonatal hypocalcemia can occur.
Big picture: calcium results integrate the bone–parathyroid–kidney–gut axis and often uncover primary hyperparathyroidism or malignancy-related processes. Read together with albumin, they forecast risks such as fractures, kidney stones, arrhythmias, and chronic kidney strain, linking day‑to‑day symptoms to long‑term outcomes.
What Insights Will I Get?
Hypercalcemia testing matters because calcium is a master signal for nerve firing, muscle contraction, heart rhythm, vascular tone, hormone release, blood clotting, and bone remodeling. When blood calcium runs high, it can disturb energy, mood and cognition, digestion, kidney water balance, and cardiovascular stability. At Superpower, we test Calcium, Corrected Calcium, and Albumin.
Calcium is the total calcium in blood, combining free (ionized) calcium and protein-bound calcium. Hypercalcemia refers to an elevation of this total or the ionized fraction. Corrected Calcium estimates what total calcium would be if albumin were normal, helping reveal the true calcium status when binding proteins are abnormal. Albumin is the main carrier protein for calcium; changes in albumin shift measured total calcium without necessarily changing the biologically active free calcium.
Together, these markers clarify stability across systems. A high true calcium load can shorten cardiac repolarization, reduce neuromuscular excitability, slow gut motility, and impair renal concentrating ability, while signaling increased bone resorption or altered hormone pathways. Corrected Calcium reduces misclassification when albumin is low or high, improving assessment of severity and physiological impact. Albumin itself informs binding capacity and oncotic pressure, helping distinguish apparent from true hypercalcemia and adding context for fluid status and protein nutrition.
Notes: Interpretation varies with age, pregnancy (hemodilution lowers albumin), acute illness, dehydration, and assay variability. Medications and conditions such as hyperparathyroidism, malignancy, granulomatous disease, and thiazide diuretics can raise calcium. Drawing conditions (tourniquet time) and timing can modestly affect total calcium.






.avif)



.svg)





.svg)


.svg)


.svg)

.avif)
.svg)










.avif)
.avif)
.avif)


.avif)
.png)


