Key Benefits
'- Detect high blood sodium (hypernatremia) early to prevent complications.
- Spot dehydration-driven imbalance from illness, heat, heavy sweating, or limited water.
- Clarify symptoms like extreme thirst, confusion, irritability, or muscle twitching.
- Guide safe rehydration and correction speed to reduce risk of brain swelling.
- Flag kidney or hormone-related causes, like diabetes insipidus or lithium-related water loss.
- Track effects of medications, tube feeds, or saline infusions on your sodium balance.
- Support pregnancy care by monitoring sodium during severe vomiting, fever, or diarrhea.
- Interpret best with serum and urine osmolality, urine sodium, glucose, and symptoms.
What are Hypernatremia
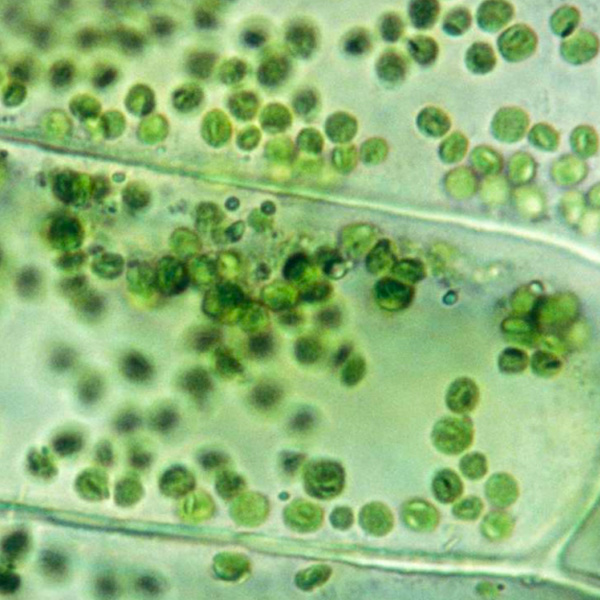
Hypernatremia biomarkers are measurements that reveal too much sodium relative to water in the blood and, crucially, why it’s happening. The central signal is blood sodium (Na+), which reflects overall tonicity (plasma osmolality) and the tendency for water to move out of cells. Paired blood and urine tests show whether the problem stems from water loss or sodium gain and how the body is reacting. Urine concentration (urine osmolality) and urine sodium indicate kidney concentrating ability and salt handling. Blood indicators of hydration and filtration (BUN and creatinine) show the toll of volume depletion, while glucose can point to osmotic diuresis that wastes water. Hormonal markers—antidiuretic hormone signaling via arginine vasopressin (AVP) or its stable proxy copeptin, and the renin-angiotensin-aldosterone system (RAAS)—reveal whether the brain and adrenal system are trying to conserve water and salt. Taken together, these biomarkers trace the path from cause to response—what drove sodium upward, how dehydrated cells may be, and whether kidneys and hormones are compensating—so care can target the underlying driver and restore water–salt balance safely.
Why are Hypernatremia biomarkers important?
Hypernatremia biomarkers—chiefly serum sodium alongside serum and urine osmolality—tell you how your body is balancing water and salt. Because sodium sets plasma tonicity, these markers predict how water shifts between blood and cells, especially in the brain, and signal kidney and hormonal responses that maintain volume and pressure.
Sodium is generally interpreted across 135–145, with health clustering near the middle. Values drifting toward either edge stress the nervous system and kidneys; pregnancy resets the “normal” point slightly lower due to physiologic hypo‑osmolality.
When values run high, water is relatively scarce or sodium is in excess. Cells dehydrate and shrink, most critically neurons, producing intense thirst, dry mouth, restlessness, confusion, muscle twitching, and seizures; cerebral bleeding can occur in severe cases. Urine that is very concentrated suggests appropriate vasopressin response to water loss (fever, diarrhea); urine that stays dilute points to diabetes insipidus. Infants and older adults are especially vulnerable because thirst and access to fluids are limited, and symptoms can be subtle (irritability in babies, delirium or falls in older adults).
When values run low, the issue is excess water relative to sodium. Cells swell, causing headache, nausea, gait instability, and seizures; the brain is again the target organ. Pregnancy normally shifts sodium lower, so mildly low readings can be physiologic there.
Big picture: sodium-related biomarkers integrate kidney concentrating ability, vasopressin and aldosterone signaling, cardiovascular volume status, and brain safety. Persistent dysnatremia—high or low—tracks with worse cognition, fractures and falls, arrhythmias, and mortality, and often unmasks renal, endocrine, or osmotic disturbances (including hyperglycemia) that merit attention.
What Insights Will I Get?
Hypernatremia biomarker testing matters because sodium sets extracellular tonicity, water distribution, brain cell volume, renal concentrating responses, and blood pressure. Hypernatremia signals a hyperosmolar state that stresses the brain and cardiovascular system and impairs cognition. At Superpower, we test Sodium.
Sodium is the principal extracellular electrolyte (cation) that sets serum osmolality. Hypernatremia means sodium concentration is elevated, almost always from water deficit relative to total body sodium, less often from sodium gain. It reflects inadequate water intake or excessive free-water loss (renal or extrarenal) or an excess hypertonic load. Rising sodium draws water out of cells, especially in the brain, creating neurologic vulnerability.
For stability and healthy function, sodium within a tight range indicates intact thirst mechanisms, antidiuretic hormone (AVP) signaling, and kidney concentrating capacity. When sodium is high, it suggests those homeostatic loops are overwhelmed or impaired. The body compensates by releasing AVP and concentrating urine, but persistent elevation implies ongoing water loss or hypertonic exposure. Clinically, this state signals cellular dehydration, potential hemodynamic instability, and stress on cognition and neuromuscular function.
Notes: Interpretation depends on chronicity (acute elevations cause more symptoms; chronic may be subtler), age (infants and older adults are more susceptible), access to water, intercurrent illness (fever, diarrhea, burns), and medications or solutions (diuretics, lithium, mannitol, hypertonic fluids, tube feeds). Pregnancy modestly lowers the osmostat. Assay method (direct vs indirect ISE) and lab-to-lab variation can influence reported values.






.avif)



.svg)





.svg)


.svg)


.svg)

.avif)
.svg)










.avif)
.avif)
.avif)


.avif)
.png)


