Key Benefits
- Spot true low calcium by correcting for albumin, not just total calcium.
- Explain numbness, cramps, tingling, or spasms that point to hypocalcemia.
- Guide urgent care if levels drop enough to affect heart rhythm or seizures.
- Clarify causes with context: vitamin D deficiency, parathyroid disorders, kidney disease, medications.
- Track recovery on calcium, vitamin D, or magnesium therapy and dietary changes.
- Protect bones by flagging persistent imbalance that accelerates bone loss and fractures.
- Support pregnancy by keeping maternal calcium adequate for fetal bone and newborn needs.
- Best interpreted with ionized calcium when albumin is abnormal or critical illness exists.
What are Hypocalcemia
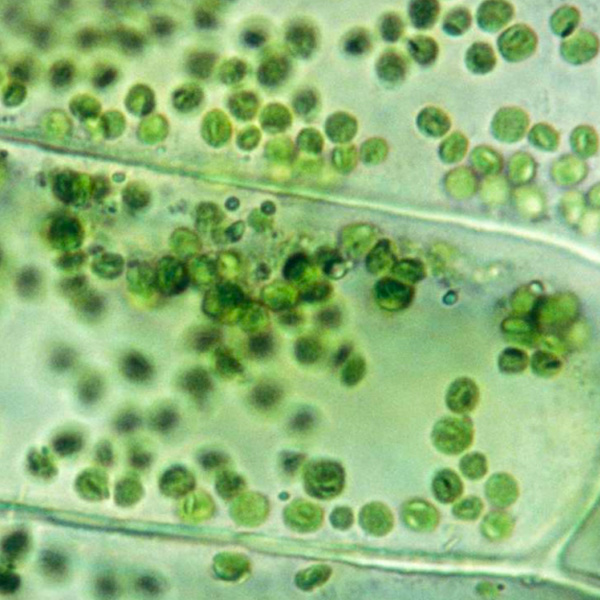
Biomarker testing for hypocalcemia reveals how your calcium-control system is working and which part is under strain. It begins with calcium itself, capturing both the total in circulation and the biologically active “free” fraction (ionized calcium). It then checks the key regulators that raise or lower calcium: the parathyroid signal (parathyroid hormone, PTH) and the vitamin D pathway, including the storage form and the active hormone (25-hydroxyvitamin D and 1,25-dihydroxyvitamin D). Supporting players clarify the terrain: the mineral cofactor that stabilizes this system (magnesium), the counterbalancing mineral that can tie up calcium (phosphate), and the main blood carrier that binds calcium (albumin). Kidney status adds context because the kidneys activate vitamin D and conserve calcium (creatinine as a kidney function marker). Read together, these biomarkers map calcium’s journey from gut and bone into blood and cells, indicating whether sensing, hormone signaling, vitamin D supply, kidney handling, or blood binding is the bottleneck. That map guides targeted, physiology-based correction of low calcium.
Why are Hypocalcemia biomarkers important?
Hypocalcemia biomarkers tell you how much biologically available calcium your nerves, muscles, heart, and blood-clotting systems can actually use. Because calcium is a key signaling ion, even small shortfalls ripple across the neuromuscular system, cardiac rhythm, and bone remodeling.
Total Calcium typically sits around 8.6–10.2, with optimal values in the middle. Albumin is usually 3.5–5.0; since much of calcium rides on albumin, low albumin can make total calcium look low when ionized (active) calcium is normal. Corrected Calcium estimates the true level by accounting for albumin; when corrected into the standard calcium range, mid-range tends to be physiologically steady. In pregnancy, total calcium often appears lower due to hemodilution and lower albumin, so corrected or ionized values better reflect status.
When calcium runs low, the body leans on parathyroid hormone and vitamin D to keep nerve and muscle thresholds stable. If these systems can’t compensate—after thyroid/parathyroid surgery, with vitamin D deficiency, kidney disease, pancreatitis, or low magnesium—neuromuscular excitability rises: tingling around the mouth and fingertips, muscle cramps, carpopedal spasms, tetany, and seizures. The heart may show a prolonged QT and arrhythmias; breathing can be affected by laryngospasm. Children may present with irritability or seizures, and chronic insufficiency can impair growth and bone mineralization.
Big picture, hypocalcemia biomarkers integrate the calcium–parathyroid–vitamin D–magnesium axis with kidney function, bone turnover, and albumin status. Tracking total, corrected, and albumin together helps distinguish true calcium lack from binding changes, clarifying risks for arrhythmias, fractures, and neurocognitive symptoms over time.
What Insights Will I Get?
Calcium is a core signaling ion for nerve firing, muscle contraction (including the heart), vascular tone, clotting, bone remodeling, and hormone/immune pathways. Low biologically active calcium (hypocalcemia) destabilizes these systems, affecting neuromuscular control, cardiac rhythm, and skeletal integrity. At Superpower, we test these specific biomarkers: Calcium, Corrected Calcium, Albumin.
Calcium (total) reflects both protein-bound and free (ionized) calcium in blood. Corrected Calcium estimates what total calcium would be if albumin were normal, helping separate true hypocalcemia from low binding protein states. Albumin is the main carrier protein for calcium; when albumin is low, total calcium falls even if ionized calcium is unchanged.
When both total and corrected calcium are low, this indicates true hypocalcemia and reduced calcium available for membrane excitability, cardiac conduction, coagulation, and bone mineral balance—raising risk for neuromuscular irritability, prolonged QT, and secondary parathyroid stress on bone. If total calcium is low but corrected calcium is normal, physiologic calcium signaling is usually preserved; the issue is reduced binding capacity from low albumin rather than a deficit of free calcium. Low albumin itself signifies altered protein synthesis or distribution (such as inflammation, liver dysfunction, or renal/gastrointestinal loss) and makes total calcium more variable, so corrected values better reflect functional stability.
Notes: Interpretation is influenced by pregnancy (hemodilution lowers albumin and total calcium), age, acute illness and pH (alkalosis lowers ionized calcium), medications (e.g., calcimimetics, anticonvulsants, diuretics), citrate from transfusions, and assay variability. Severe hypoalbuminemia or high globulins can bias total calcium; ionized measures best reflect biologic calcium under these conditions.






.avif)



.svg)





.svg)


.svg)


.svg)

.avif)
.svg)










.avif)
.avif)
.avif)


.avif)
.png)


