Key Benefits
- Check kidney protein loss and heart risk in nephrotic syndrome.
- Spot severe protein loss through low albumin and total protein levels.
- Explain swelling and weight gain by linking hypoalbuminemia to fluid retention.
- Flag atherogenic lipids: high LDL, triglycerides, and ApoB signal added risk.
- Guide treatment intensity, including statins, RAAS blockers, diuretics, and nutrition changes.
- Track recovery; rising albumin and falling ApoB and triglycerides indicate improvement.
- Prompt clot-risk review when albumin is very low, especially with immobility.
- Best interpreted with urine protein-to-creatinine ratio, eGFR, and blood pressure.
What are Nephrotic Syndrome
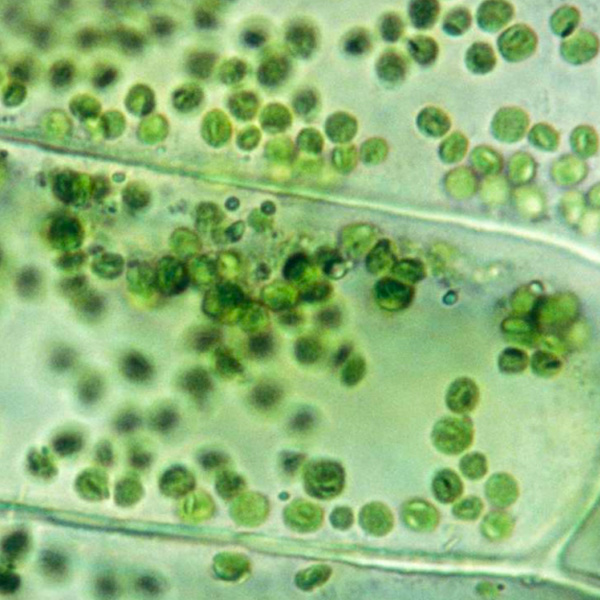
Nephrotic syndrome biomarkers are the body’s measurable signals that the kidney’s filter is damaged and leaking protein, and they map both the leak and its ripple effects. The core marker is protein in the urine (albuminuria/proteinuria), which comes directly from the glomerular filter (podocytes and basement membrane). Blood albumin mirrors how much protein is escaping (hypoalbuminemia), while the liver’s response shows up as changes in blood lipids (hyperlipidemia) — a downstream footprint of the same leak. Kidney function indicators (serum creatinine and estimated filtration) show how well the kidneys are clearing wastes, even when the leak is the main problem. Electrolytes and measures of fluid balance reflect salt and water retention that drives swelling (edema). Cause-finding biomarkers — such as specific autoantibodies in primary disease (PLA2R) or complement patterns in immune conditions — help pinpoint the trigger and guide therapy. Together, these urine and blood markers let clinicians detect nephrotic syndrome, gauge severity, anticipate complications like clotting (thrombosis), and monitor response as the barrier heals or worsens.
Why are Nephrotic Syndrome biomarkers important?
Nephrotic syndrome biomarkers track how a leaky kidney filter reshapes the whole body. When glomeruli spill protein into urine, blood loses key proteins that hold fluid in vessels and carry hormones and lipids. The liver responds by making more lipoproteins, tipping cholesterol and triglycerides upward. These shifts touch the cardiovascular, immune, endocrine, and clotting systems—so following albumin, total protein, LDL, triglycerides, and ApoB shows both kidney injury and its systemic ripple effects.
Albumin is usually about 3.5–5.0, and total protein about 6–8; in health, both sit in the middle-to-upper part of their ranges. LDL and triglycerides are healthiest toward the lower end (LDL under 100, triglycerides under 150), and ApoB commonly spans roughly 60–120, with lower generally better for risk.
When values fall—especially albumin and total protein—it signals heavy urinary protein loss and falling oncotic pressure. Fluid shifts into tissues, causing ankle swelling, abdominal bloating, and weight gain; children often show puffy eyelids on waking. Fatigue, muscle cramps, and foamy urine are common. Very low proteins can also reduce carrier-bound hormones and vitamins, amplifying hypothyroid-like symptoms or low vitamin D effects. If LDL, triglycerides, or ApoB are unusually low in this setting, it may reflect remission or, less commonly, poor nutrition or liver synthesis problems. In pregnancy, low albumin can intensify edema and magnify hemodynamic stress.
Markedly high LDL, triglycerides, and ApoB in nephrotic syndrome reflect hepatic overproduction of atherogenic particles as protein is lost, increasing long-term cardiovascular and thrombotic risk, even when albumin is low. Big picture: these biomarkers integrate kidney barrier health with liver metabolism, vascular risk, immunity, and endocrine transport, helping anticipate complications like edema, infection, clotting, atherosclerosis, and chronic kidney disease progression.
What Insights Will I Get?
Nephrotic syndrome biomarker testing shows how a leaky glomerular filter disrupts fluid balance, transport proteins, and lipid metabolism. These shifts affect energy handling, vascular integrity, immune protein reserves, and hormone/drug transport—key determinants of cardiovascular risk and overall system stability. At Superpower, we test Albumin, Total Protein, LDL, Triglycerides, and ApoB.
Albumin is the main plasma protein maintaining oncotic pressure; in nephrotic syndrome it falls because it is lost in urine. Total Protein (albumin plus globulins) drops when albumin and some immunoglobulins are lost. LDL rises as the liver overproduces lipoproteins to compensate for protein loss. Triglycerides rise from increased VLDL production and reduced clearance. ApoB, the structural protein on atherogenic particles, increases in parallel and quantifies particle number more directly than cholesterol alone.
Together, Albumin and Total Protein reflect vascular stability and transport capacity; lower levels signal edema risk, altered pharmacokinetics, and reduced immune protein buffering. LDL, Triglycerides, and ApoB indicate the intensity of nephrotic lipid remodeling and atherogenic burden; higher values map to greater endothelial stress and impaired energy trafficking. Improvement is typically marked by rising Albumin/Total Protein and normalization of ApoB-containing lipoproteins.
Notes: Interpretation is influenced by acute inflammation (albumin is a negative acute-phase reactant), hydration status, fasting status (triglycerides), pregnancy (hemodilution and physiologic hyperlipidemia), age, and medications such as corticosteroids and estrogens that raise lipids. Lab methods differ (calculated versus direct LDL; ApoB assay variability), and monoclonal proteins can elevate Total Protein independent of nephrotic loss.






.avif)



.svg)





.svg)


.svg)


.svg)

.avif)
.svg)










.avif)
.avif)
.avif)


.avif)
.png)


