Key Benefits
- Confirm or rule out vitamin B12 deficiency that can cause anemia and nerve injury.
- Spot macrocytic anemia by linking high MCV and low hemoglobin to B12 lack.
- Clarify red cell changes: higher MCH, normal MCHC, and high RDW suggest deficiency.
- Differentiate B12 from folate deficiency to choose the right replacement therapy.
- Explain fatigue, numbness, memory changes by linking blood indices with low B12.
- Protect nerves by replacing B12 promptly and avoiding folate-only therapy with low B12.
- Support pregnancy planning and fertility by ensuring adequate B12 and folate stores.
- Track treatment response as hemoglobin rises and MCV, RDW normalize over weeks.
What are Vitamin B12 Deficiency
Biomarkers for vitamin B12 deficiency show whether your body has enough B12 and whether cells are actually using it to make DNA and protect nerves. They capture both supply and function. Total circulating B12 (serum vitamin B12) reflects the overall pool in blood. The fraction that can be delivered into cells, the “active” form (holotranscobalamin), reflects cellular availability. Downstream signals reveal functional shortfall inside cells: methylmalonic acid (MMA) accumulates when a B12‑dependent enzyme for fat metabolism stalls (methylmalonyl‑CoA mutase), and homocysteine accumulates when B12 is lacking for one‑carbon recycling and methylation (methionine synthase). Together, these markers indicate whether B12 is reaching tissues and performing its roles in red blood cell formation and myelin maintenance. In practice, this testing helps confirm true tissue deficiency, detect problems early—sometimes before blood count or nerve symptoms appear—and monitor recovery once B12 is restored. In short, B12 deficiency biomarkers translate a hidden cellular need into measurable signals that guide timely, targeted care.
Why are Vitamin B12 Deficiency biomarkers important?
Vitamin B12 deficiency biomarkers show whether your cells can divide properly and your nerves can maintain their insulation. Because B12 powers DNA synthesis and myelin repair, these markers reflect blood health, brain and nerve integrity, oxygen delivery, and energy metabolism across the whole body.
Most labs consider hemoglobin normal in the low‑ to mid‑teens for men and slightly lower for women; feeling best usually tracks with the mid‑to‑upper part of that range. MCV typically spans 80–100, with optimal toward the low‑to‑mid 90s; MCH 27–33 and MCHC 32–36 perform best in the middle. RDW is normally about 11–15, and lower is steadier. Vitamin B12 often reads 200–900, with mid‑to‑high appearing more reliable. Folate is commonly 5–20, and mid‑to‑high is desirable.
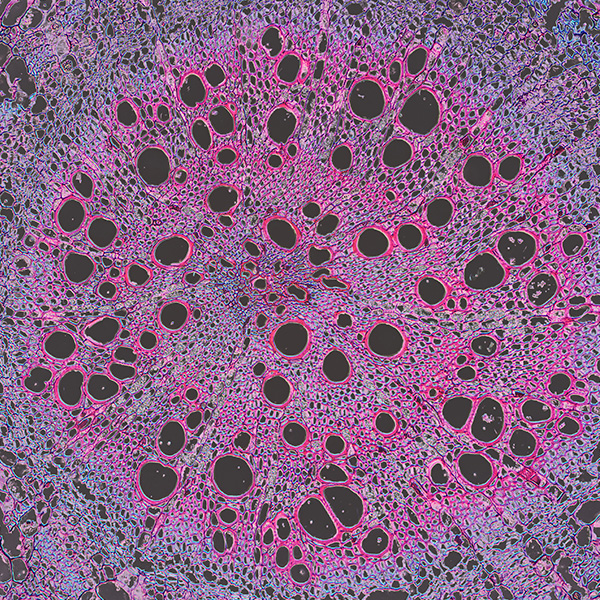
When B12 is low, DNA synthesis slows, marrow releases large, fragile red cells: hemoglobin falls, MCV and MCH rise, MCHC stays normal, and RDW widens. You may feel fatigue, shortness of breath, palpitations, pale skin, a sore tongue, numbness or tingling, balance trouble, vision changes, memory fog, and low mood. Children can show poor growth or developmental delay. Women, with lower baseline hemoglobin, can manifest anemia sooner; older adults are more vulnerable due to absorption issues. Adequate folate may partially normalize blood indices while nerve injury from B12 lack continues.
Big picture, these biomarkers connect gut absorption, hematology, methylation (homocysteine), and neurocognition. Tracking them helps identify risk, gauge severity, and monitor recovery, reducing long‑term risks like irreversible neuropathy, cognitive decline, falls, and adverse pregnancy outcomes.
What Insights Will I Get?
Vitamin B12 powers DNA synthesis, methylation, and myelin maintenance—core processes for red blood cell formation, energy delivery, cognition, and cardiovascular health. Disruption shows up first in blood-cell dynamics. At Superpower, we test these specific biomarkers: Hemoglobin, MCV, MCH, MCHC, RDW, Vitamin B12, Folate.
Hemoglobin reflects oxygen-carrying capacity; B12 deficiency can reduce it by impairing erythropoiesis. MCV (cell size) typically rises in megaloblastic states from faulty DNA replication. MCH (hemoglobin per cell) often appears higher because cells are larger, while MCHC (hemoglobin concentration) is usually normal. RDW (size variation) increases as the marrow releases unevenly developed cells. Vitamin B12 measures cobalamin status; low values suggest deficiency. Folate shares the one‑carbon pathway; low folate mimics B12 deficiency, and normal folate can normalize blood indices while neurologic risks from low B12 persist.
Together, these markers show the stability of oxygen transport and one‑carbon metabolism. Adequate B12 and folate with normal MCV, MCHC, and RDW signal robust, synchronized red‑cell production. Macrocytosis with high RDW and falling hemoglobin indicates unstable DNA synthesis and ineffective erythropoiesis. Low B12, with or without anemia, points to impaired methylation and potential neurologic vulnerability, while discordant patterns help distinguish isolated B12 lack from mixed causes.
Notes: Interpretation is influenced by pregnancy (hemodilution), age, liver disease, hypothyroidism, alcohol use, and acute illness. Medications such as metformin, proton pump inhibitors, nitrous oxide, and some anticonvulsants affect B12 or folate status. Assay methods and binding proteins vary, so results should be interpreted in clinical context.






.avif)



.svg)





.svg)


.svg)


.svg)

.avif)
.svg)










.avif)
.avif)
.avif)


.avif)
.png)


