You fuel up the car, breathe city air, sit next to a smoker at a game, and feel fine — but your body keeps the score. The N‑Acetyl Phenyl Cysteine (NAP) test translates invisible benzene exposure into a simple number you can track. Think of it as a receipt your body prints after processing benzene. Curious how that receipt gets made, what it means, and how to use it?
What This Test Actually Measures
Plain-English definition
The NAP test measures N‑acetyl‑S‑phenyl‑L‑cysteine in urine, a “mercapturic acid” your liver and kidneys make after your body encounters benzene. In other words, it detects a specific benzene metabolite that reflects recent exposure and how effectively you’re conjugating it for excretion.
How it gets into the body
Benzene primarily enters through inhalation from sources like gasoline vapor, traffic exhaust, and tobacco smoke. It’s volatile, moves quickly from lungs to blood, partitions into fat, and is metabolized in the liver. Unlike persistent pollutants, benzene doesn’t stockpile for months — it’s processed and cleared on the order of hours to days, though biologic effects can outlast the exposure. Want to see the fingerprint of yesterday’s air?
What sample you’ll provide
A spot urine sample. Many labs prefer first‑morning voids or end‑of‑shift samples for occupational monitoring. Results often come in micrograms per liter or corrected to creatinine (micrograms per gram creatinine) to account for hydration. Ready to catch a 24–48‑hour snapshot?
How the Test Works
Collection and timing
Collection is straightforward: urinate into a clean container, cap, and ship promptly per the kit’s instructions. For consistency, aim for the same time of day on repeat tests. Hydration dilutes urine, so creatinine‑corrected results help normalize values; try to keep your fluid intake similar each time. If you’re assessing workplace exposure, pair a pre‑shift and post‑shift sample to capture changes across the workday. Curious whether a commute or refueling stop is showing up in your data?
Most labs quantify NAP using liquid chromatography coupled to tandem mass spectrometry (LC‑MS/MS). This technique isolates the compound and measures it with high specificity and low detection limits. That precision is why NAP is considered a more specific benzene biomarker than alternatives influenced by diet.
What the number represents
Your value represents the amount of N‑acetyl‑S‑phenyl‑L‑cysteine excreted in urine — a product of benzene first oxidized to benzene oxide and then conjugated with glutathione before final N‑acetylation. Because the metabolite’s half‑life is short, results reflect recent exposure, generally the past day or two. So if you topped off the tank or were around smoke yesterday, would you expect a bump today?
What the Results Mean
Reference intervals vs. personal context
Population ranges are reference points, not personal goals. Levels vary by smoking status, urban vs. rural air, occupational exposures, ventilation, and the timing of your last exposure. Labs report different units and use different methods, so compare results within the same lab when trending. In large population surveys, smokers tend to sit several‑fold higher than nonsmokers, which highlights how context shapes interpretation. How might your daily routine explain your position on the curve?
Pattern recognition
Elevated NAP with high cotinine — a nicotine metabolite — often points to tobacco smoke exposure (active or secondhand). A spike after refueling, commuting windows, or shop time around solvents suggests inhalation from fuel and garage air. If another benzene biomarker like trans,trans‑muconic acid rises while NAP stays low after a preservative‑heavy meal, diet may be confounding the former while NAP stays more benzene‑specific. Seeing repeat elevations tied to a specific weekday or activity?
Follow-up testing
Because the window is short, retesting after a suspected source change helps confirm directionality. For occupational settings, serial pre‑/post‑shift pairs clarify whether the workplace is the driver. For lifestyle sources, retest one to two weeks after altering ventilation, storage of fuels, or exposure to smoke to see if levels trend down. Wouldn’t it be useful to watch the line move rather than guessing?
Key Systems Affected
Nervous system
High benzene exposure can cause headaches, dizziness, and impaired concentration through central nervous system effects. At lower environmental levels, acute neurologic symptoms are less typical, but sensitive individuals may still notice fatigue or mental “fog” after intense exposures like time in a poorly ventilated garage. If symptoms cluster after specific exposures and NAP rises in tandem, that’s a clue. Do your brain “off days” map to your exposure map?
Liver and detox pathways
The liver’s cytochrome P450 2E1 converts benzene to benzene oxide, which is either detoxified by glutathione conjugation to form NAP or diverted to other metabolites. This process can nudge oxidative stress, and markers like gamma‑glutamyl transferase may correlate with increased detox demand. Alcohol use can induce CYP2E1, potentially shifting metabolic patterns. Does your liver’s workload show up in both exposure and stress signals?
Kidneys and filtration
Kidneys excrete NAP into urine. Hydration and renal function influence uncorrected concentrations, which is why creatinine correction is often used. In chronic kidney disease, interpretation can be skewed by altered creatinine or excretion dynamics. Could kidney context be blurring an otherwise clear exposure picture?
Endocrine and metabolism
Benzene is not classically framed as a leading endocrine disruptor, but systemic oxidative and inflammatory stress can ripple into metabolic regulation. In high‑exposure settings, broader physiologic strain may interact with hormonal signaling and energy balance, though data at low environmental levels are limited. Are your metabolic markers steady while exposure fluctuates, or do they move together?
Common Sources of Exposure
Environmental and household
Typical sources include gasoline vapor during refueling, attached garages that share air with living spaces, urban traffic, and indoor air impacted by tobacco smoke. Small engines — lawn equipment, generators, scooters — stored or run in enclosed spaces can raise indoor benzene. Old adhesives or solvents may contribute in specific settings. Could your garage or commute be louder than you think?
Dietary and occupational
Diet is not a major benzene driver for most people, though rare contamination can occur. Occupational risks persist in petroleum refining, fuel distribution, some manufacturing, and auto repair environments where fuel vapor accumulates. Historical high‑risk industries included printing and shoe manufacturing before modern controls. Does your job or hobby put you near fuels, solvents, or poorly ventilated workspaces?
Clues from history
Ask yourself: Do you refuel several times per week? Park in an attached garage below a bedroom? Spend hours in traffic with windows down? Live with a smoker or frequent outdoor venues with concentrated smoke? Use or store gasoline‑powered devices indoors? Specific patterns like “Monday spikes” can point to weekly routines. Which habit is your likely culprit?
Detoxification and Elimination
Physiology 101
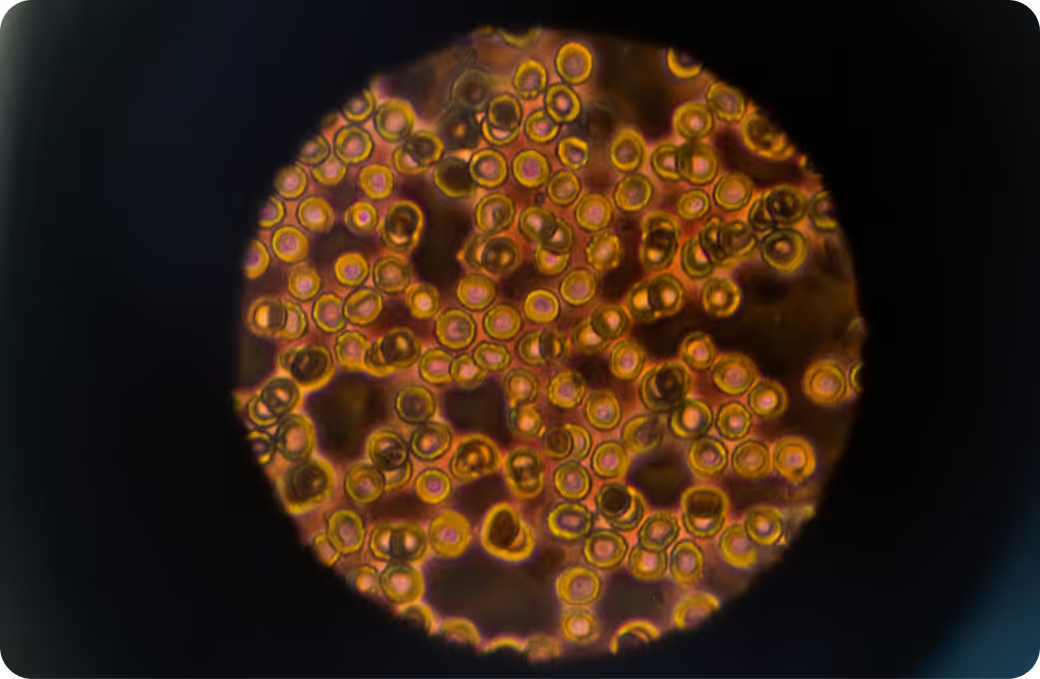
The path looks like this: benzene inhaled → oxidized by CYP2E1 to benzene oxide → conjugated with glutathione via glutathione‑S‑transferases → processed to S‑phenylcysteine → N‑acetylated to N‑acetyl‑S‑phenyl‑L‑cysteine (NAP) → excreted in urine. Most of this unfolds within hours, giving the test its short exposure window. With a timeline that quick, how recent was your last meaningful exposure?
Systems that support clearance
Glutathione availability, GST enzyme capacity, N‑acetyltransferase activity, renal blood flow, and urinary excretion all shape how much NAP appears. The redox system recycles glutathione using enzymes that depend on micronutrients and mitochondrial energy supply. When these systems are humming, the body tags and moves benzene metabolites efficiently. Are your clearance gears well oiled or catching?
Why responses vary
Genetics (such as GSTM1/GSTT1 deletions), CYP2E1 activity, nutrient status, alcohol use, co‑exposures, age, and underlying illness can all shift detox speed and pathway balance. Two people breathing the same air may produce different amounts of NAP. That’s why your baseline matters more than your neighbor’s. How does your biology personalize your exposure story?
Biomarker Correlations
Functional context from broader labs
A complete blood count can reveal marrow signals tied to benzene at higher exposures, such as lower white blood cell or neutrophil counts. High‑sensitivity C‑reactive protein offers a window into systemic inflammation. Liver enzymes, especially GGT, can hint at detox strain. Nicotine exposure markers like cotinine help attribute source when NAP is elevated. Which companion markers sharpen your interpretation?
Nutrient cofactors and capacity
Glutathione synthesis relies on cysteine, glycine, and glutamate, while recycling depends on riboflavin‑dependent enzymes and adequate NADPH. Selenium supports peroxidase defenses, and folate/B12 status contributes to nucleotide synthesis and DNA repair when oxidative stress rises. These aren’t prescriptions — they’re the biochemical levers that influence detox capacity. Do your nutrient‑linked systems suggest resilience or bottlenecks?
Interpreting together
Pair a rise in NAP with a stable, healthy CBC and steady inflammatory markers, and the blip may reflect a transient exposure with minimal physiologic ripple. See repeated elevations alongside subtle downward drift in neutrophils, and the pattern warrants attention in context. Add cotinine to sort tobacco smoke from other sources. With multiple data points, are you seeing random noise or a clear signal?
Optimal vs. Normal
Population ranges
Reference ranges describe what’s common in a population, not what’s ideal for you. Labs differ in units and cutoffs, and population surveys consistently show higher values in smokers than nonsmokers. Because hydration skews raw concentrations, creatinine‑corrected values often give a cleaner comparison. Where do your numbers sit relative to people with similar lifestyles?
Longevity-oriented targets
For benzene metabolites, many clinicians aim for “as low as reasonably achievable” rather than a rigid cutoff, given the compound’s toxicology and occupational history. The goal is practical reduction, not perfection. If your value can move from the upper percentiles toward the lower, isn’t that direction what matters most?
Trend over time
A single data point is a snapshot; a series is a story. Repeat testing under similar conditions lets you see if changes stick. If an intervention is truly cutting exposure, the curve should bend and stay low rather than yo‑yo. Would a simple trendline make your choices clearer?
Why Testing Is Worth It
From mystery to measurement
Headaches after refueling, fatigue after garage time, or no symptoms at all — it’s all guesswork until you measure. The NAP test turns invisible air exposures into numbers you can plot. Once quantified, patterns emerge and decisions get easier. Isn’t it easier to change what you can see?
Guiding remediation
Elevated NAP that tracks with smoke exposure suggests a smoking‑related source, while spikes after refueling point to fuel vapor or ventilation issues. That distinction focuses effort on the right lever: source reduction, work‑practice changes, or environmental controls. With clear attribution, what would you prioritize first?
Prevention and baseline
Establishing your personal baseline is powerful. It helps you detect new exposures quickly and verify that improvements stick over seasons, jobs, or moves. When your baseline is solid, any shift stands out early. What would a reliable baseline unlock for you?
Limits, Caveats, and Smart Use
Scope and specificity
NAP is a specific benzene metabolite, but it reflects recent exposure only. It won’t capture distant past exposures or cumulative lifetime risk. Tobacco smoke can dominate the signal in smokers and those with secondhand exposure, so source context matters. Are you reading the number through the right lens?
Not a diagnosis
This test does not diagnose disease. It quantifies exposure and biotransformation. Health effects depend on dose, duration, co‑exposures, and individual susceptibility, and medical evaluation requires a broader clinical picture. Does your data fit with your clinical context?
Nonlinearity and thresholds
Small changes at the low end can be meaningful for trend tracking, while large swings after intense exposures may normalize quickly as the metabolite clears. In other words, response isn’t always linear across all ranges or timeframes. Are you comparing apples with apples across tests?
Make Your NAP Result Actionable with Superpower
Exposure data gets powerful when you connect it to how your body responds. Pairing your NAP result with physiologic markers — from inflammation to detox capacity — turns a single number into a narrative about resilience, bottlenecks, and real‑world change.
See your exposure in context. Layer the NAP test with Superpower’s 100+ biomarker panel to map sources, track trends, and watch your biology adapt in real time. Ready to turn an invisible exposure into a plan you can follow?